Over the past couple years I have thought about posting many times but was never in the right mindset or motivated when the thought came. I realized that as much as this is to share my journey it is also for me to record life and express myself. I am coming to understand that I have to want to write for me more than anything and am trying not to feel pressure to say something important but to just share life, no matter how inconsequential it feels. I am also realizing that sometimes it is difficult emotionally to share what has/is happening and I need to make sure that I prioritize my health (mental and physical) above all else. With that said, I fully intend to go back and share everything that has happened in the last couple crazy years but it may take a little while for me to feel ready.
I recently learned that July is disability pride month. While there is also a disability awareness month (as well as months to raise awareness about many specific conditions/diseases), this is a time to embrace our disabilities and share who with are with our conditions, not in spite of them. The reason July is the month of celebration is because on July 26, 1990 the Americans with Disabilities Act (ADA) was passed ensuring rights for those of us that live with disabilities. Having learned this I have been thinking a lot about what it means to be proud of myself and the way my disability shapes me, as well as to accept and love the life that I lead as a disabled woman.
It has taken me a long time to accept that I am a disabled woman (and I still sometimes struggle to admit this). When I first started showing symptoms my biggest priority was to figure out what was causing them, solve the problem and get back to ‘normal’ life. Admitting that I am disabled means in large part accepting that this is who I am and this is the life I lead. It also means learning to love and celebrate the things that I do and the person I am, living this life that is so completely different from anything I ever envisioned or hoped my life would be.
I still have many days (or weeks or months) where all I want is to go back to the person I used to be, before I was sick. However, I am learning more and more to see the positives in the person that being sick has made me and the way that I have grown since this journey began. This doesn’t mean that I love being sick or am fighting any less to gain more independence and stability, but, it does mean that I am coming to appreciate the strength and depth that I have gained as a result.
In honor of disabilty pride month I would like to take a moment to really love the disabled person I am and communicate what being proud of this means for me. I do want to say before I dive in that not every disabled person has the same journey and that my experience and feelings in no way reflect disabled people as a whole. Each disabled person has their individual opinions and views on what disability pride looks like. This is mine.
Before becoming disabled I was an educated, somewhat naive, young adult who had somewhat positive views about the world as a whole and was convinced that I was going to do big things that would change the world in big ways. I had my whole life planned out and there was nothing that was going to stand in my way or alter my plan. I thought I knew exactly who I was meant to be and who I was. For the beginning of this crazy health journey (which was several years) I felt like I was falling behind on my plan and was becoming more and more distressed that my life had been derailed and was going to be harder and harder to get back on track to the way that it was ‘supposed’ to be. I was constantly approaching things from the perspective of how quickly I could get back to the ‘normal’ that I expected my life to be.
As the years progressed and my health continued to decline I became despondent that my life was slipping through my fingers and that I had completely failed. Every decision I made and ever challenge that was thrown my way just emphasized how far I was getting from the ‘right path’ that I was supposed to be on. If I am completely honest I still go through periods of time (sometimes frequently) that I feel so discouraged and feel like a complete failure. I felt like the situation I was in was in some way a reflection of the person I was or was tied to how motivated or hard working I was. There was (and sometimes still is) nothing that could convince me that my health was not my ‘fault’ and that it had nothing to do with my character or actions. I have even gone through periods where I felt like I wasn’t doing the sick girl thing right either. As if there was a right way to handle my disorders and that I was somehow failing at that too.
As my health deteriorated to the point that I was facing death I couldn’t get past the thought that I had failed at life and that I was a pointless waste. I was convinced that I had achieved nothing meaningful and that made me completely worthless as a human being. Even when things started to (very slowly and very minimally) improve I was convinced that it didn’t matter as I had missed my window to ‘make’ my life matter and that there was nothing I could do to matter. I watched my peer group lead their lives and just knew that they were better than me because of the things that were happening in their lives. I even watched other disabled people and felt like I was not as ‘good’ at being disabled as they were. I often felt incredibley alone, as if there was no one who could possibly understand how much of a failure I was. Every development with my health pushed me further into the despair that I would never amount to anything. *I want to note that the people closest to me never made me feel less than in any way and often went out of the their way to let me know how special and valuable I was. They constantly tried to make me see that I wansn’t a failure or a useless waste of life. Unfortunately, often these assurances did nothing to improve my outlook or change the way I felt (which is no reflection on the people around me).
I got so low that I didn’t even want to engage with the measures that were improving my life and didn’t care if I was miserable. It felt like everything I tried or did was pointless because nothing could change the long term outcome and nothing could give me back the life that I had lost. As more time passed it became more and more clear the gap between what my life looked like and the lives of those I had once been close to was rapidly expanding. I watched as those that were younger experienced and ‘surpassed’ the things that were supposed to have happened in my life. I frequently felt like I was not even worth talking to or being around anymore as everyone else had great lives without me and that I had nothing to contribute in any way. Everything about me felt like another reason why I was not valuable and was a burden on the world around me.
If I am being completely transparent I still struggle with thoughts of being worthless and a burden. I frequently fall into the trap of comparisson, both to the people around me and to the life that I thought I was supposed to lead. Even the triumphs sometimes feel like stupid things to celebrate and I feel like a fool for getting excited about the small things in life and the ‘minor’ things I accomplish. I often find it challenging to remember that my journey may not be like other people’s but it is not less than and that the things I accomplish are no less valuable because they are different than the accomplishments of others. It is hard work to remember to see my worth in things other than the physical contributions I have not made and to find value simply in the person that I am.
As I have spent more time in the past couple weeks really thinking on what it means to be proud of my disabled self I have come to a few conclusions. Deep down I truly love the person that I am today, not in spite of the disabilities that I live with but WITH and because of them. I am learning to accept the ‘broken’ parts of me as things that make me who I am and things that without I would be a completely different human. I am also working to love the things that help me live life and function to the best of my ability as well as embracing the difficult things that have shaped my story.
Here are some of those things.(in no particular order)
- First, (and this is a difficult one for me recently) I am proud of my scars. This includes the ones from my numerous injuries as well as the ones from my many procedures and surgeries. At times I feel self conscious about the scars on my face from falls, the scars on my abdomen from feeding tubes and surgeries, and the scars on my chest from my central lines. I am learning to see my scars as reminders of my strength and of the times that I have overcome. I am also learning to appreciate the surgical ones as marks of the times when science helped save and better my life. I am trying to be proud to show what makes me me through the physical scars that I carry and to love the marks that show the journey I am on.
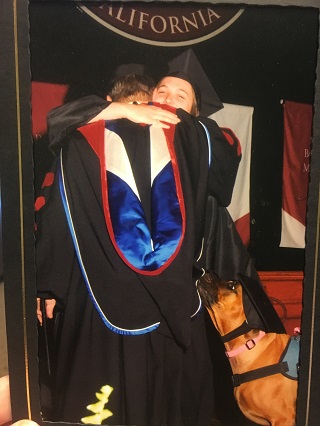
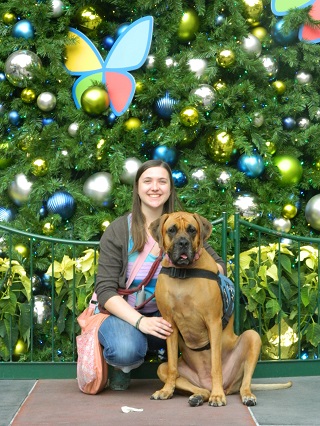
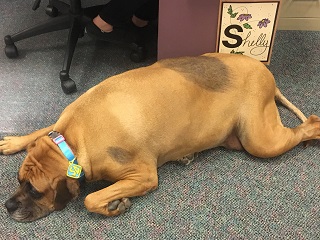
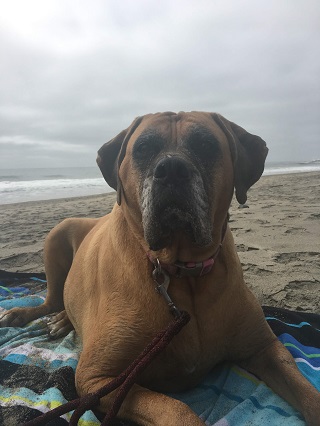
- Second, I am proud to show the medical equipment that helps me function and is a piece of me. I am proud of my central line and the way that it helps me get the fluids that I need to be able to live the life that I lead. I am proud of my wheelchair because it allows me to engage in the world in ways I may not otherwise be able to. I am incredibly proud of Apollo, my service dog, and the work that he is doing to help me being a more independent individual. I am learning to not be ashamed of the noise that my pumps make and the added challenge that requiring medical equipment carries (especially when travelling).
- Third, I am learning to be proud of the things I accomplish. The physical activity I work hard to achieve. The way I engage with the world and work to support those around me. The animals I have shared life with and worked to impact through my actions. The contributions I make in the lives of my family and friends just through being there as I am.
- Finally, I am proud to share my life. I am proud to be a friend and support for those around me. Having POTS (and gastroparesis, autonomic neuropathy, migraines, etc.) is a huge part of who I am. It has showed me how much strength and resilience I have. It has taught me to appreciate life in a different way. It has showed me who my true friends and support system are, those who really stick around when things are tough. It teaches me every day the things that truly matter and is constantly helping me see what truly makes me happy and fufilled in life. There are times (often) when I wish I wasn’t disabled and that I could go through life without these burdens. However, I am learning to see these things not as burdens at all but as pieces of me that make me who I am and are shaping the person I am becoming!
To wrap things up, while I may struggle with accepting who I am and may struggle to see the value I have with my disability, in the end I am working hard to say … I am PROUD to be a disabled woman!!